Why is it important to make a frugal monitoring device for premature babies?
Some figures
Goal 3 of the United Nations sustainable development goals is to ensure healthy lives and promote well-being for all at all ages. One of the targets for this is to end preventable deaths of newborns and children under 5 years of age by 2030. In particular, one aim is for all countries to reduce neonatal mortality to at least as low as 12 per 1,000 live births. In 2015, the UN Inter-agency Group for Child Mortality Estimation estimated an average number of 21 per 1000 neonatal deaths in developing regions. In comparison, developed regions have on average 3 neonatal deaths per 1000 live deaths. Overall, neonatal deaths account for 45% of under-five mortality worldwide. [Child Mortality Report (2015) ]
In 2010, complications of preterm birth were identified as the single largest direct cause of neonatal deaths, responsible for 35% of them. They are also the second most common cause of under-five deaths, after pneumonia. As such, both the reduction of preterm birth and the mortality reduction among babies born preterm are essential issues in the pursuit of the United Nations sustainable development goals. [Born too soon (2012) ]
Preterm births and possible complications
In 2012, a collective of organisations has published Born Too Soon , a global action report on preterm birth. While the figures cited need updating, the trends observed show that the described phenomena and problematics still stand.
Preterm births are defined according to gestational age, the measure of the duration of a pregnancy as the time elapsed since the woman's last normal menstrual period. Babies born alive before 37 weeks of gestational age are preterm. Below 32 weeks, babies are labelled very preterm (about 10% of all preterm births) and below 28 weeks, extremely preterm (about 5% of all preterm births).
Of the 15 million children born preterm each year, only one third have access to full intensive care or neonatal care units. The remaining babies are either born and cared for at home (5.6 million) or are born in health facilities that face limited space, staff and equipment. Very and extremely preterm children, of course, require the most care. Therefore, they have the highest mortality rate in low- and middle- income countries. However, even babies born after 32 weeks of pregnancy face specific challenges.
Preterm babies have higher risks of hypothermia, hypoglycemia, hypoxia, feeding difficulties, severe infections, respiratory issues, jaundice, brain injuries, retinopathy and anaemia. Some of those issues can be addressed easily with the proper training and low-cost material. For example, Kangaroo Mother Care, a skin-to-skin technique of newborn care, helps keep the baby warm enough. Overall, it was estimated in 2012 that 3 out of 4 neonatal death linked to preterm complications could be avoided even without access to neonatal intensive care services.
Existing baby monitors: reassure the parents
There are already a number of monitors for newborns on the market. Most of them are not specifically fitted to preterm babies' needs. They are also designed to reduce parents' fears and give them a feeling of control rather than addressing an actual medical need. Most work with a mobile tracking app and possibilities for integration of other smart devices. They keep track of a range of markers from the most useful like temperature to the most accessory like room light levels. In addition to this, their price range -minimum 100$- and format -some require constant new purchases as the baby grows- make it clear that they target high-income populations.
There is, however, one device worthy of attention in the context of preterm death in low- and middle-income countries: Bempu is a bracelet that constantly measures the body temperature of the wearer. It is intended for preterm babies and other newborns with complications. It does not rely on a mobile app for function but instead rings an alarm when the temperature drops. This way, the caretakers can take steps to stop hypothermia before it has negative consequences. Bempu is developed and distributed in India. It is sold to hospitals and clinics to be distributed to parents of at-risk newborns. Its cost, around 50$, makes it relatively affordable to health infrastructure but is still quite high for individuals of low-income regions.
To sum it up, reducing neonatal deaths and, in particular, those of preterm babies is a global goal. We believe that wearable devices have the potential to support parents in their care of preterm babies and that most of the existing solutions are not adapted to the needs of low-income regions. This is the central motivation for our project.
Our project: a frugal wearable alert for temperature, heart-rate, oximetry and skin colour
In addition to the review of the reports made available by NGOs, we have initiated a survey process to better pinpoint the needs and desires of the various populations that could benefit from a project like ours. We have started to circulate a questionnaire in French and Indian neonatal medical environments. The first responses have helped us define our precise targets and goals. We hope to receive more answers from health professionals and parents in the following weeks.
Target
With the support of ZMQ , a social enterprise based in India, we have decided to focus our project on the families of preterm babies in low-income regions. We target specifically moderate and late premature babies with no severe health issues, who are born at home or sent home before they have reached the normal development of a newborn.
Our goal is twofold: to provide the parents and other caretakers with means to monitor the health of their baby, and to guide their reactions when the baby needs specific care.
We do not aim to replace parental care or health clinics! We wish to create a device that can both alert to specific problems and propose an adequate response, in regions where health care and education are sparse.
Choice of measures
Our choice of the vitals monitored by our device was driven by two considerations: whether the measure could be made continuously by a connected wearable on the baby, and whether an action could be taken by the caretaker outside of an intensive neonatal care unit.
We have selected four markers: temperature, oxygen blood saturation, skin colour and heart-rate.
Temperature monitoring is especially important for preterm babies who do not have access to a neonatal care unit. All newborn have difficulties regulating their temperature for the first few hours of their life, but babies born preterm can struggle with it for far longer. Hypothermia appears to be a central problem in global mortality of preterm babies. Yet, it can be easily addressed with swaddling and skin-to-skin (Kangaroo care) methods. This question is already the focus of a lot of health initiative, and the Kangaroo care technique is widely promoted.
By monitoring the temperature, the device can also alert the caretakers when the child is feverish. Fever is dangerous for preterm babies, both in itself as a too high body temperature might damage the forming organs, and because it is the symptom of another problem. Parents alerted to their baby's fever can take steps to reduce this fever, and get bring their child to a local health facility if the fever persists or is too high.
Many preterm babies have respiratory complications. A drop in oxygen blood saturation reflects respiratory distress and needs to be addressed immediately. Local health workers can be trained to perform basic neonatal resuscitation.
Skin colour can reflect a number of problems in babies, but only two are common and involve a widespread colour change. Jaundice is a very common condition in newborn and has higher occurrence rates in preterm babies. If the skin turns yellow, the parents should bring their child to a health care centre so it can receive the appropriate treatment. Unlike oxygen depletion, this is not an immediate emergency. However, if the skin turns blue, it is the sign that oxygen levels have been depleted long enough to have an impact and the caretakers should seek professional help as fast as possible.
Heart-rate is more of an emergency indicator: if the heart slows down significantly or stops, the child requires emergency health care. However, it is not uncommon for newborns, and especially preterm babies, to have their heart stop beating for a few seconds. In this case, Kangaroo care is suggested to promote a regular heartbeat.
Design plan
The design of our device can be split into three main aspects: the electronics, the physical design of the objects and the design of the interactions.
Electronics
The main electronics that are needed include a heart-rate, SP02 and a temperature sensor. A colorimetric sensor may be added depending on the time that we have. The different sensors have certain specifications that need to be followed in order to obtain a device which is secure and small enough for the child.
Specifications:
- as small as possible: Each component must be maximum 1.2 cm wide and 4 mm thick.
- low power: Each component must run on max 3.6V
- cheap as possible
To transfer data and run the code we will need a microchip and 2 ESPs as internet connection may not be accessible parts of different countries.
These specifications will allow the product to be accessible to populations with low income. Furthermore, batteries will be able to last the required time (1-2 months ) in order to help the parents.
Object design
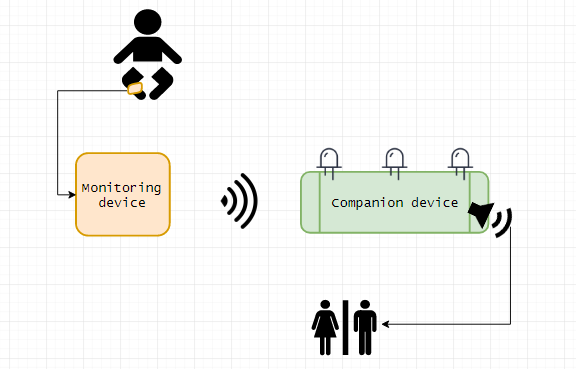
Our project relies on two objects: a wearable for the baby and a companion object to alert the parents when something is wrong and advise them on the reaction.
The design of the baby accessory is both more constrained and more important for proper function.
In order for the measurements to be precise, the sensors need to be maintained in an appropriate position. For example, heart rate sensors need to be in contact with the skin.
We have identified some important issues due to the delicate nature of the users. The skin of preterm babies is often very sensitive. Materials need to be chosen according to this, and the design of the wearable has to protect the skin from abrasion by the electronic component. Simultaneously, the accessory should be adjustable: newborns grow fast and all of the preterm baby's measurement are expected to grow greatly during the time they will wear our device.
There is also the social significance of accessories to consider. We have been advised to favour the leg, the ankle or the foot to place our monitoring device, as accessories worn to the wrist or the head often have cultural meanings.
In addition to this, as a wearable, the device should be washable and at least slightly waterproof. It should be sturdy enough to be worn permanently in varying environments for up to a few months.
Our main lead currently is to place the sensors on a sock-like elastic band around the foot and the other electronic components in a tight bracelet. The sensors will come in contact with the skin thanks to windows in the textile material of the foot bracelet.
The companion object should be as mobile as possible. As for the wearable device, it should be safe around young children. We are currently iterating on a geometrical shape with a speaker and light indicators on the top and indicative instructions of the sides.
Interactions
To interact between the monitoring device and the companion device a method accessible to all with and without internet connection must be used. [more information on the companion device interactions with the parents will be published when we obtain the required knowledge from health professionals ]
 Emma Barme
Emma Barme